White matter disease, also known as leukoaraiosis or white matter hyperintensities, is a condition characterized by damage to the white matter in the brain. It’s often associated with aging and conditions such as hypertension, diabetes, and cerebral small vessel disease.
Life expectancy with white matter disease can vary significantly depending on various factors such as the severity of the disease, overall health of the individual, and presence of other medical conditions. In many cases, white matter disease is not immediately life-threatening itself, but it can increase the risk of cognitive decline, stroke, and other neurological complications, which can affect life expectancy.
It’s essential for individuals diagnosed with white matter disease to work closely with healthcare providers to manage underlying conditions and adopt lifestyle changes that can help mitigate risk factors. Regular monitoring and appropriate treatment can help improve quality of life and potentially extend life expectancy.
What are the causes and risk factors of white matter disease?

White matter disease, also known as leukoaraiosis or white matter hyperintensities, refers to changes in the brain’s white matter seen on MRI or CT scans. It’s commonly associated with aging, but several factors can contribute to its development:
- Getting Older: White matter disease is more common in older people.
- High Blood Pressure: When blood pressure is too high for a long time, it can hurt the brain’s blood vessels and cause white matter disease.
- Diabetes: If someone has diabetes that’s not managed well, it can damage blood vessels in the brain, leading to white matter disease.
- Blocked Arteries: Fatty deposits can block the arteries, making it hard for blood to flow to the brain. This can cause white matter disease.
- Smoking: Smoking is bad for the blood vessels, which can lead to white matter disease.
- High Cholesterol: Too much cholesterol can also hurt the blood vessels, increasing the risk of white matter disease.
- Family History: Sometimes, it can run in families.
- Other Brain Problems: If someone has had strokes before or has certain heart problems, it can increase the risk of white matter disease.
- Being Overweight: Being very overweight can also make someone more likely to get white matter disease.
- Unhealthy Lifestyle: Not eating well, not exercising, drinking too much alcohol, or being too stressed can also contribute to white matter disease.
How does white matter disease progress and what symptoms are associated with it?
White matter disease, also known as leukoaraiosis or small vessel ischemic disease, typically progresses slowly over time. It is characterized by the deterioration or damage to the white matter in the brain, which consists of nerve fibers covered in a fatty substance called myelin. This damage is often caused by the decreased blood flow to small blood vessels deep within the brain.
The progression of white matter disease can vary from person to person, but generally, it tends to worsen gradually over years rather than rapidly. The symptoms associated with white matter disease can also vary widely depending on the extent and location of the damage. Common symptoms may include:
Cognitive Impairment
White matter disease can lead to difficulties with thinking, memory, and other cognitive functions. This can manifest as problems with attention, executive function, processing speed, and memory recall.
Motor Symptoms
Some individuals may experience changes in motor function, such as weakness, clumsiness, or difficulties with coordination and balance.
Mood and Behavior Changes
White matter disease can also affect mood regulation and behavior. Symptoms may include depression, apathy, anxiety, irritability, or emotional instability.
Gait Abnormalities
Walking may become more challenging due to balance problems or weakness in the legs.
Urinary Symptoms
In some cases, white matter disease can lead to urinary symptoms such as urgency, frequency, or incontinence.
Visual Changes
Damage to certain areas of white matter can result in visual disturbances, including blurred vision, double vision, or difficulty with visual processing.
How is white matter disease diagnosed and what is the prognosis?
Diagnosing white matter disease typically involves a combination of medical history review, physical examination, and diagnostic tests. Here are the primary methods used for diagnosis:
Medical History and Physical Examination
The healthcare provider will ask about symptoms, medical history, and risk factors such as hypertension, diabetes, smoking, and cardiovascular disease.
A neurological examination may also be conducted to assess cognitive function, motor skills, and reflexes.
Imaging Tests
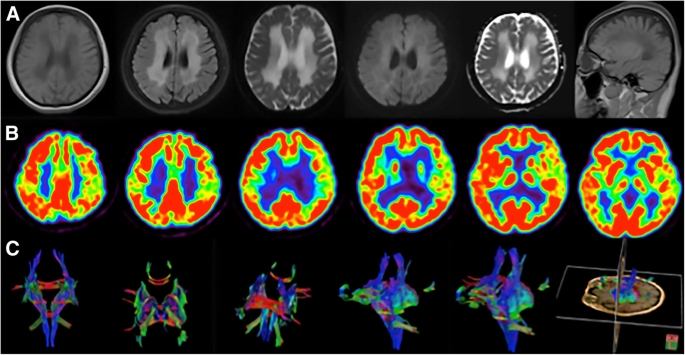
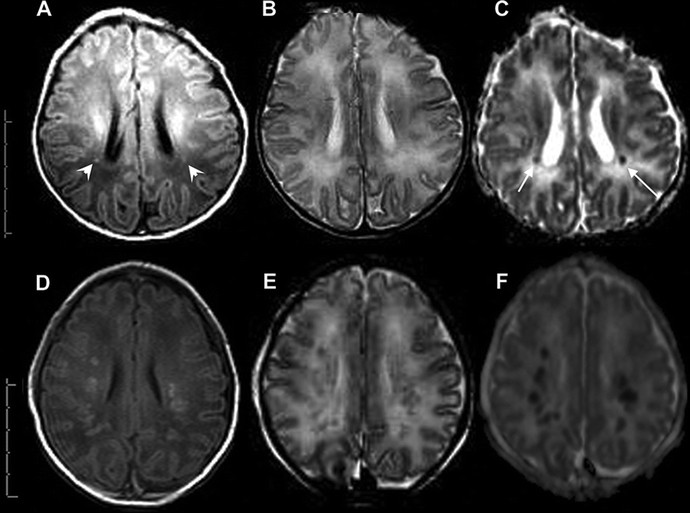
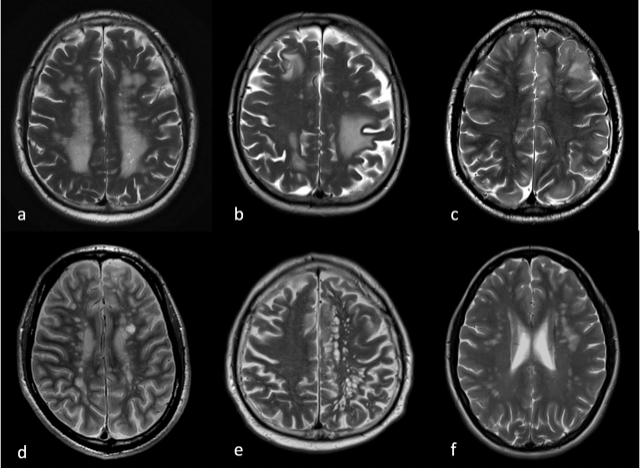
Imaging studies such as magnetic resonance imaging (MRI) are crucial for diagnosing white matter disease. MRI can reveal changes in the brain’s white matter, including areas of hyperintensity or lesions. These changes are indicative of white matter damage or ischemic injury.
MRI can also help differentiate white matter disease from other conditions that may present with similar symptoms, such as multiple sclerosis.
Other Tests
Additional tests may be ordered to evaluate the underlying causes or contributing factors of white matter disease. These may include blood tests to assess for risk factors like high cholesterol or diabetes, as well as tests to evaluate cardiovascular health.
The prognosis for individuals with white matter disease can vary widely depending on factors such as the severity of symptoms, underlying health conditions, and response to treatment. In general:
- White matter disease tends to progress slowly over time. However, the rate of progression can vary among individuals.
- The prognosis may be influenced by factors such as the extent of white matter damage, the presence of other medical conditions, and lifestyle factors such as diet and exercise.
- While white matter disease itself is not typically life-threatening, it can significantly impact cognitive function, mobility, and quality of life.
- Treatment focuses on managing symptoms, addressing underlying risk factors, and preventing further progression of the disease. Lifestyle modifications, medication, and rehabilitation therapies may be recommended to help manage symptoms and improve overall function.
- Regular monitoring by healthcare professionals is essential to track disease progression, adjust treatment as needed, and provide support to individuals and their caregivers.
Final Words
Managing the effects of white matter illness on life expectancy requires an understanding of the condition. Its causes, symptoms, diagnosis, and available treatments have all been explained to us. People can take proactive measures to control their health by being aware of risk factors including aging and ailments like diabetes and hypertension. Maintaining a healthy lifestyle and assessing oneself on a regular basis can assist increase life expectancy and enhance quality of life. Overall, the best possible outcomes for patients suffering from white matter illness depend on early discovery and all-encompassing care.