White matter disease, also referred to as leukoaraiosis or small vessel ischemic disease, is a complex neurological condition characterized by damage or abnormalities in the white matter of the brain. This condition typically arises due to diminished blood flow to the small blood vessels in the brain, resulting in the degeneration of white matter tissue. Understanding the nuanced progression of white matter disease is paramount for early detection, effective management, and tailored intervention strategies. In this article, we embark on a thorough examination of the four distinct stages of white matter disease, shedding light on their defining characteristics, observable symptoms, and profound implications for both patients and caregivers.
Stage 1: Mild White Matter Changes
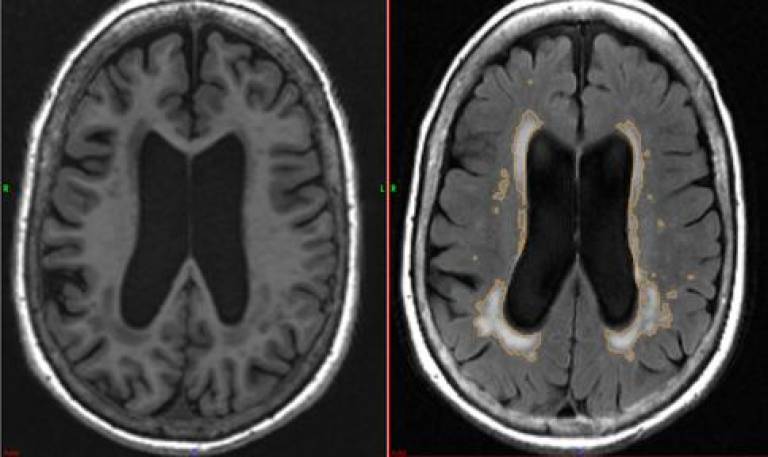
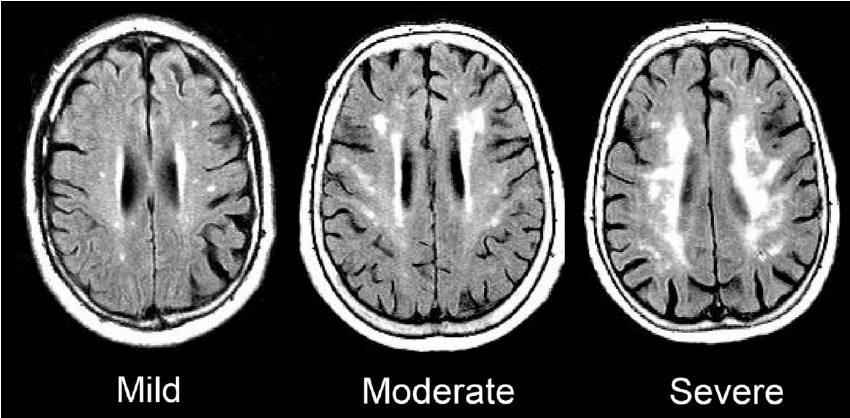
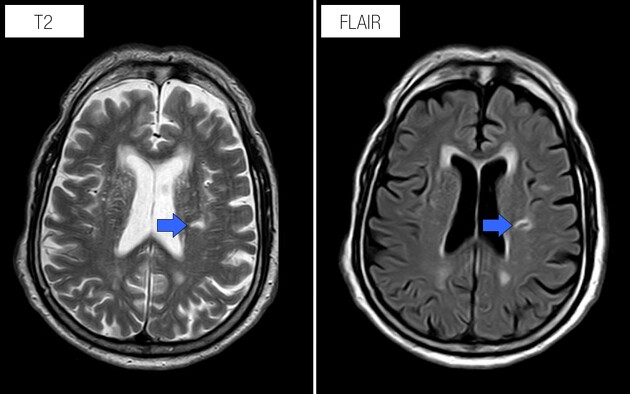
The inaugural stage of white matter disease unveils subtle alterations in white matter structure, often discernible through advanced imaging techniques like magnetic resonance imaging (MRI).
Despite these early anomalies, individuals may remain largely asymptomatic or attribute minor manifestations such as sporadic headaches or mild memory lapses to other factors.
Nonetheless, this stage underscores the critical importance of medical evaluation and vigilant monitoring to discern the trajectory of the disease and instigate preemptive measures to stall its progression.
Stage 2: Moderate White Matter Changes
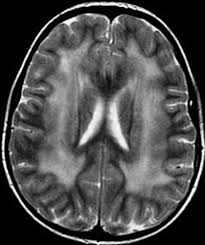
As the disease advances to its intermediate phase, the scope of white matter abnormalities expands, accompanied by a concomitant escalation of symptoms. Cognitive impairment becomes more evident, with individuals grappling with memory deficits, attentional lapses, and compromised executive function. Mood fluctuations may ensue, encompassing symptoms like depression, apathy, or emotional volatility. Additionally, mild motor disturbances may emerge, such as an unsteady gait or challenges with fine motor control.
While these symptoms may not yet severely impair daily functioning, they serve as poignant indicators necessitating comprehensive neurological assessment and tailored management strategies.
Stage 3: Severe White Matter Changes
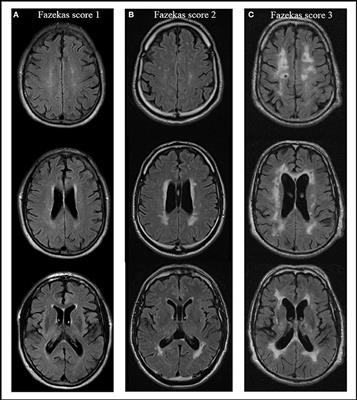
In the penultimate stage of white matter disease, the detrimental impact on white matter integrity becomes markedly pronounced, precipitating a significant decline in cognitive faculties and functional independence. Memory deficits intensify, affecting both short-term and long-term memory domains.
Language comprehension and expression may become compromised, accompanied by episodes of confusion or disorientation. Profound alterations in personality and behavior may surface, posing considerable challenges for both individuals and caregivers.
Motor symptoms may progress to the extent that mobility is substantially impaired, warranting assistance with activities of daily living. During this critical phase, robust caregiver support and targeted interventions aimed at bolstering cognitive function and enhancing quality of life become imperative.
Stage 4: End-Stage White Matter Disease
The final stage of white matter disease heralds a profound descent into cognitive decline, severe motor impairment, and loss of autonomy. Individuals may find themselves in a state of profound dependency, necessitating full-time care either in specialized facilities or within the confines of their own homes, facilitated by trained caregivers.
Communication may become severely compromised, exacerbating the individual’s sense of isolation and vulnerability. While medical interventions and supportive measures can ameliorate symptoms and optimize comfort, the prognosis for those grappling with end-stage white matter disease remains daunting.
Conclusion
White matter disease represents a formidable neurological adversary, posing formidable challenges for patients, caregivers, and healthcare providers. By unraveling the complexities of its four progressive stages, individuals can gain a deeper understanding of its evolving symptomatology, proactively seek medical evaluation and support, and make informed decisions regarding treatment modalities and care pathways.
Early detection coupled with proactive management is paramount in navigating the formidable terrain of white matter disease, fostering optimal outcomes, and preserving functional independence to the greatest extent possible.