White matter disease, or leukoaraiosis, demands a multifaceted treatment approach. Managing underlying conditions like hypertension and diabetes is key, often involving medication and lifestyle adjustments. Medications such as antihypertensives and statins help control risk factors. Lifestyle changes like a balanced diet, exercise, and stress management are crucial. Physical therapy aids in improving mobility and balance, while cognitive rehabilitation addresses cognitive impairments. Symptomatic treatment may be necessary for specific symptoms like depression or urinary incontinence. Regular monitoring through imaging and clinical evaluations ensures timely adjustments to the treatment plan. Collaboration with healthcare providers is essential for a tailored approach to managing white matter disease and maintaining quality of life.
How does white matter disease develop?

White matter disease, also known as leukoaraiosis or white matter hyperintensities, develops due to damage or abnormalities in the white matter of the brain. White matter is composed of nerve fibers covered in myelin, a fatty substance that acts as insulation and facilitates communication between different regions of the brain.
The exact cause of white matter disease is not always clear, but it is commonly associated with aging and conditions that affect blood flow to the brain. Some potential factors contributing to its development include:
Aging
As people age, changes occur in the brain’s blood vessels, making them more susceptible to damage. This can lead to reduced blood flow to the white matter, resulting in injury or loss of function.
Hypertension (High Blood Pressure)
High blood pressure can damage blood vessels throughout the body, including those in the brain. Chronic hypertension can lead to small vessel disease, disrupting blood flow and causing damage to the white matter.
Diabetes
Diabetes can also damage blood vessels, increasing the risk of white matter disease. High blood sugar levels can lead to inflammation and oxidative stress, contributing to vascular damage in the brain.
Atherosclerosis
Atherosclerosis, the buildup of plaque in the arteries, can restrict blood flow to the brain, leading to white matter damage.
Smoking
Smoking is a risk factor for vascular disease, including white matter disease. The toxins in cigarette smoke can damage blood vessels and reduce blood flow to the brain.
Hypercholesterolemia (High Cholesterol)
High levels of cholesterol can contribute to the development of atherosclerosis, further increasing the risk of white matter disease.
Genetic Factors
Some genetic factors may predispose individuals to white matter disease or conditions that increase the risk of its development.
What are the diagnostic methods for white matter disease?

Diagnostic methods for white matter disease typically involve a combination of clinical assessment, neuroimaging techniques, and evaluation of risk factors. Here are the main diagnostic approaches:
Medical History and Physical Examination
The doctor will take a detailed medical history, including asking about symptoms such as cognitive changes, gait disturbances, or other neurological symptoms. A physical examination may also be conducted to assess neurological function.
Neuroimaging
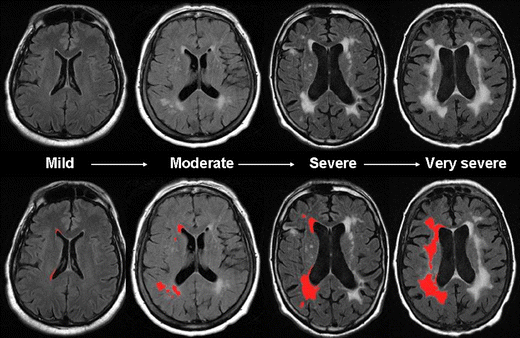
- MRI (Magnetic Resonance Imaging): MRI is the primary imaging modality used to diagnose white matter disease. It can detect changes in the brain’s white matter, such as hyperintensities or areas of demyelination. MRI can also help differentiate white matter disease from other conditions with similar symptoms.
- CT (Computed Tomography): CT scans may be used to detect severe white matter changes, but MRI is generally more sensitive for detecting subtle changes associated with white matter disease.
Cerebral Angiography
In some cases, cerebral angiography may be performed to assess the blood vessels in the brain and identify any abnormalities or blockages that could contribute to white matter disease.
Blood Tests
Blood tests may be done to assess risk factors such as cholesterol levels, blood sugar levels (for diabetes), and markers of inflammation.
Cognitive and Neuropsychological Testing
Cognitive and neuropsychological assessments may be conducted to evaluate memory, attention, executive function, and other cognitive domains affected by white matter disease.
Electroencephalogram (EEG)
EEG may be used to assess electrical activity in the brain and detect abnormalities that could indicate white matter disease or other neurological conditions.
Lumbar Puncture (Spinal Tap)
In some cases, a lumbar puncture may be performed to analyze cerebrospinal fluid for signs of infection, inflammation, or other abnormalities.
What are the treatment options for white matter disease?
Treatment for white matter disease aims to manage symptoms, address underlying conditions, and slow down the progression of the disease. While there’s no cure, several approaches can help improve daily life. Managing conditions like high blood pressure, diabetes, and high cholesterol is crucial. Medications like blood thinners may be prescribed to prevent clotting and improve blood flow.
Therapies such as physical therapy can help with mobility and strength. Occupational therapy focuses on daily tasks, while speech therapy may aid in communication and swallowing. Healthy lifestyle changes, like a balanced diet and regular exercise, play a key role too. Supportive care and counseling are vital for both patients and caregivers.
Working closely with healthcare providers to create a personalized treatment plan can make a significant difference in managing the condition and maintaining quality of life.
Final Words
Treating white matter disease requires a comprehensive approach that addresses its various aspects. Understanding the condition, its causes, and diagnostic methods is crucial for effective management. Treatment options include medications, therapy, lifestyle modifications, and experimental treatments.
Additionally, providing support and care for individuals with white matter disease and their caregivers is essential for improving quality of life. Looking ahead, continued research and advancements offer hope for better outcomes in the future.
