Microangiopathic changes in white matter refer to alterations in the small blood vessels within the white matter of the brain. These changes can be observed through imaging techniques such as MRI scans.
These alterations are often associated with small vessel disease (SVD), which involves damage to the small blood vessels in the brain. Common causes of microangiopathic changes include hypertension, diabetes, aging, and other vascular risk factors.
These changes can lead to a variety of neurological symptoms, depending on their severity and location. They may contribute to cognitive decline, gait disturbances, and increased risk of stroke and dementia. Management typically involves addressing underlying vascular risk factors and may include medications to manage blood pressure, diabetes, and cholesterol levels.
What causes microangiopathic changes in white matter?
Microangiopathic changes in white matter typically refer to pathological alterations in the small blood vessels within the brain’s white matter. These changes can be caused by various underlying conditions, including:
Hypertension (High Blood Pressure)
Chronic high blood pressure can lead to damage and thickening of the small blood vessels in the brain, causing microangiopathy. The vessels may become narrow or blocked, leading to reduced blood flow and oxygen delivery to the white matter.
Diabetes Mellitus
Diabetes can damage blood vessels throughout the body, including those in the brain. High blood sugar levels can cause inflammation and thickening of the vessel walls, leading to microangiopathy.
Cerebral Amyloid Angiopathy (CAA)
This condition involves the accumulation of amyloid protein in the walls of the brain’s blood vessels, particularly in the elderly. CAA can lead to vessel fragility and eventual rupture, causing microbleeds and other vascular changes in the white matter.
Small Vessel Disease (SVD)
SVD encompasses various conditions affecting the small blood vessels in the brain. These conditions can include arteriolosclerosis (thickening and hardening of arteriole walls), lipohyalinosis (deposition of lipids in vessel walls), and fibrinoid necrosis (necrosis of vessel walls due to deposition of fibrin). These changes can collectively lead to microangiopathic alterations in white matter.
Ischemic Changes
Chronic reduced blood flow to the brain due to small vessel disease or other causes can lead to ischemic changes in the white matter. Lack of oxygen and nutrients can result in damage to the white matter, manifesting as microangiopathy on imaging studies.
Other Factors
Other factors such as aging, smoking, hyperlipidemia, and genetic predispositions can also contribute to microangiopathic changes in white matter.
How do microangiopathic changes affect white matter integrity?
Microangiopathic changes can profoundly impact white matter integrity in several ways:
Disruption of Blood Flow
Microangiopathy can lead to narrowing, occlusion, or rupture of small blood vessels supplying the white matter. This disruption of blood flow deprives the white matter of oxygen and nutrients, leading to ischemia (lack of blood supply). Ischemia can result in tissue damage, white matter lesions, and loss of myelin integrity.
Hypoperfusion
Even when blood flow is not completely blocked, microangiopathic changes can reduce perfusion (blood flow) to the white matter. Chronic hypoperfusion can lead to chronic ischemia and progressive damage to white matter structures.
White Matter Lesions
Microangiopathy often manifests as white matter lesions on neuroimaging studies such as MRI. These lesions can vary in size and appearance, and they may represent areas of ischemia, demyelination, gliosis (scar tissue formation), or microbleeds. Over time, these lesions can disrupt the structural integrity of the white matter, impairing its function.
Axonal Damage
The white matter contains axons, which are the long fibers that transmit signals between different parts of the brain. Microangiopathic changes can lead to axonal injury and degeneration, impairing communication between brain regions and disrupting neural networks.
Cognitive Impairment
White matter integrity is crucial for efficient communication between different brain regions involved in cognitive functions such as memory, attention, and executive function.
Damage to the white matter due to microangiopathy can lead to cognitive impairment, including problems with memory, processing speed, and executive function.
Risk of Stroke
Severe microangiopathic changes can increase the risk of ischemic stroke, especially if they involve large areas of white matter or affect critical blood vessels supplying the brain.
What are the clinical symptoms of microangiopathic changes?
Microangiopathic changes in the brain’s white matter can cause various symptoms depending on how much and where they happen. Some common signs include problems with memory, thinking, and decision-making. People might also have trouble moving smoothly or feel weak. Sometimes, they might feel sad or anxious more often.
Vision might get blurry or sometimes they might have headaches. Feeling dizzy or having trouble keeping balance could also happen. It’s possible for these changes to make peeing more difficult too. Not everyone with these changes feels symptoms, though. Sometimes, doctors find them by accident during tests for other reasons. Seeing a doctor is important if someone notices these symptoms to figure out what’s going on and what to do about it.
How are microangiopathic changes diagnosed?
Microangiopathic changes in the brain’s white matter are often diagnosed through a combination of medical history, physical examination, and imaging studies. If a person shows symptoms like memory problems, difficulty moving, or vision changes, a doctor may suspect microangiopathic changes and ask about their medical history, including any conditions like high blood pressure or diabetes. During a physical exam, the doctor might check for signs of neurological problems.
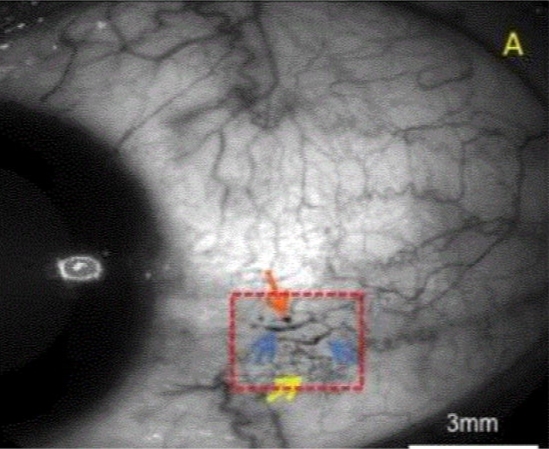
Imaging studies, especially magnetic resonance imaging (MRI) of the brain, are crucial for diagnosing microangiopathic changes. MRI can reveal the presence and extent of white matter lesions characteristic of microangiopathy. These lesions often appear as bright spots on certain MRI sequences, indicating areas of tissue damage or abnormal blood flow. Sometimes, additional imaging techniques like magnetic resonance angiography (MRA) or computed tomography (CT) scans may be used to assess the blood vessels and identify any underlying vascular abnormalities.
In some cases, other tests such as blood tests to check for risk factors like high cholesterol or diabetes, or cognitive assessments to evaluate memory and thinking abilities, may be performed to help with diagnosis and management.
Overall, diagnosing microangiopathic changes involves a thorough evaluation by a healthcare professional, often including a combination of medical history, physical examination, and imaging studies to determine the cause and extent of the changes and to guide appropriate treatment and management strategies.
Final Words
Microangiopathic changes in white matter can lead to various neurological symptoms like memory problems and difficulty walking. It’s important to identify and manage the underlying causes such as high blood pressure and diabetes. By taking steps to control these risk factors, we can potentially slow down the progression of these changes and improve quality of life. Early diagnosis and treatment are key to preventing further damage and reducing the risk of complications like stroke and dementia.
