Microangiopathic diseases encompass disorders affecting small blood vessels, leading to organ damage and various symptoms. Thrombotic thrombocytopenic purpura (TTP) and hemolytic-uremic syndrome (HUS) are notable examples, characterized by blood clot formation in microvessels, potentially affecting organs like the brain and kidneys. Diabetic microangiopathy, prevalent in diabetes, results from chronic high blood sugar levels, leading to complications such as retinopathy and neuropathy.
Treatment involves managing underlying causes and symptoms, with approaches including clot prevention, blood pressure control, and glycemic management. Supportive therapies target complications like kidney failure and neurological issues. Overall, understanding and addressing the underlying vascular abnormalities are crucial in managing microangiopathic diseases and mitigating organ damage.
Types of Microangiopathic Diseases
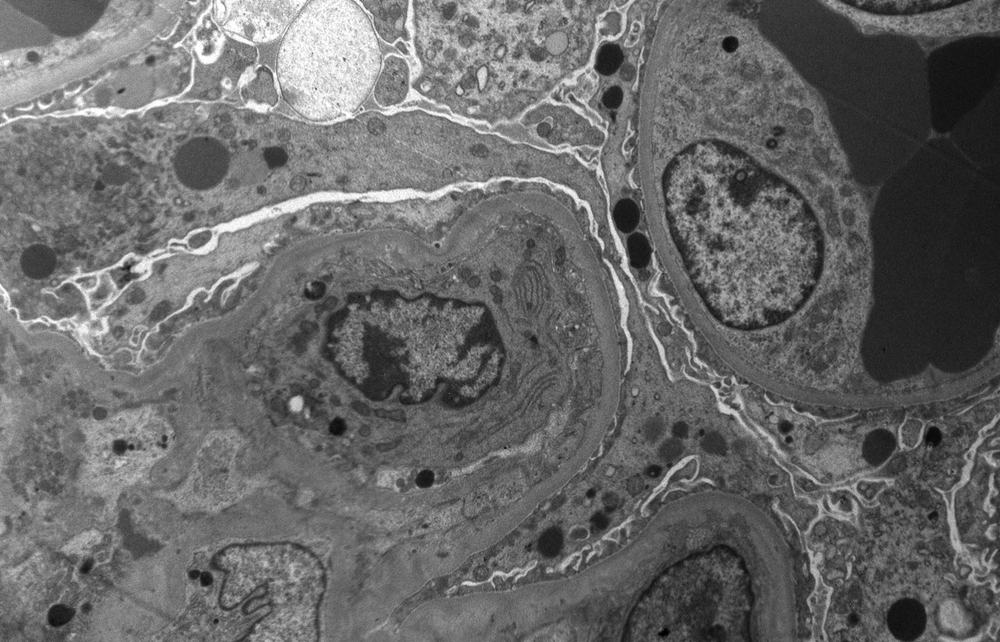
Microangiopathic diseases are conditions that affect the small blood vessels (microvessels) in various parts of the body. These diseases can lead to damage or dysfunction of these tiny blood vessels, which may cause a range of symptoms depending on the affected organs. Some common types of microangiopathic diseases include:
Thrombotic thrombocytopenic purpura (TTP)
TTP is characterized by the formation of small blood clots throughout the body, which can lead to organ damage due to reduced blood flow.
Symptoms may include fever, weakness, confusion, and abnormal bleeding such as bruising or petechiae (small red or purple spots on the skin).
TTP is often caused by a deficiency in an enzyme called ADAMTS13, which is responsible for breaking down a protein involved in blood clotting.
Hemolytic uremic syndrome (HUS)
HUS involves the formation of blood clots in the small blood vessels, particularly in the kidneys.
It is often preceded by an infection, typically with strains of E. coli bacteria that produce toxins damaging to blood vessels.
Symptoms may include abdominal pain, diarrhea (which may be bloody), vomiting, and signs of kidney failure such as decreased urine output and swelling.
Disseminated intravascular coagulation (DIC)
DIC is a complex disorder characterized by the widespread activation of the clotting cascade, leading to the formation of blood clots throughout the body.
This excessive clotting can consume clotting factors and platelets, leading to bleeding complications such as easy bruising, mucosal bleeding, and, in severe cases, organ failure.
DIC can occur as a secondary complication of various underlying conditions, including sepsis, trauma, cancer, and certain obstetric complications.
Scleroderma
Scleroderma is an autoimmune disease characterized by the excessive production and accumulation of collagen, leading to thickening and hardening of the skin and connective tissues.
In some forms of scleroderma, such as systemic sclerosis, the small blood vessels can be affected, leading to symptoms such as Raynaud’s phenomenon (cold-induced color changes in the fingers or toes), skin ulcers, and involvement of internal organs such as the lungs, kidneys, and digestive tract.
Diabetic microangiopathy
Long-term diabetes can lead to damage of the small blood vessels, particularly in the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), and nerves (diabetic neuropathy).
Diabetic retinopathy can lead to vision problems, including blindness, due to damage to the blood vessels in the retina.
Diabetic nephropathy is a leading cause of kidney failure and can result in proteinuria (excess protein in the urine) and hypertension.
Diabetic neuropathy can cause symptoms such as numbness, tingling, and pain in the extremities, as well as gastrointestinal symptoms and sexual dysfunction.
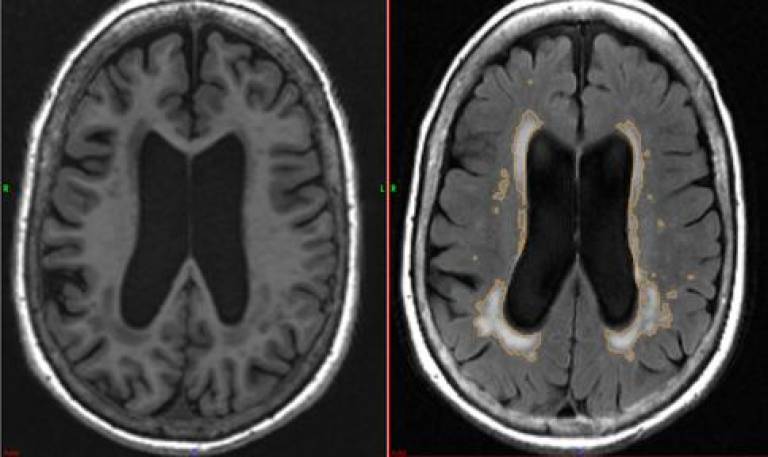
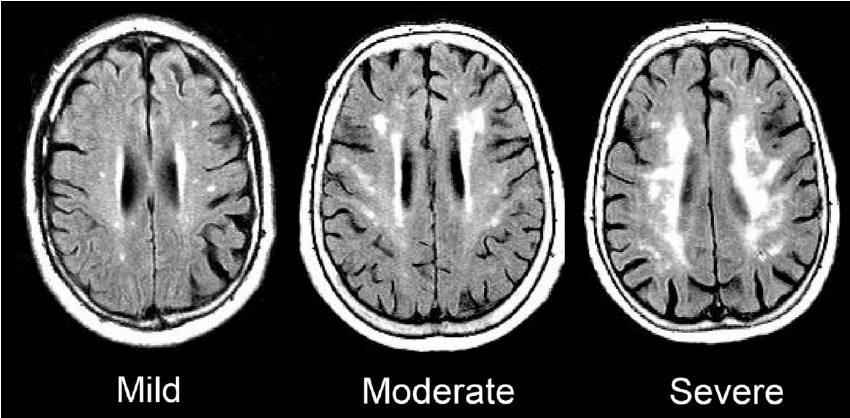
Cerebral microangiopathy
Cerebral microangiopathy encompasses various conditions affecting the small blood vessels in the brain.
Small vessel ischemic disease, a common form of cerebral microangiopathy, is characterized by the narrowing and blockage of small arteries in the brain, leading to reduced blood flow and ischemic damage.
Symptoms may include cognitive decline, such as memory loss and difficulty with executive function, as well as an increased risk of stroke.
Systemic lupus erythematosus (SLE)
Lupus is an autoimmune disease that can affect multiple organs and tissues, including the skin, joints, kidneys, and blood vessels.
In some cases, lupus can lead to inflammation of the small blood vessels (vasculitis), causing tissue damage and organ dysfunction.
Vasculitis in lupus can manifest with symptoms such as skin rashes, joint pain, kidney inflammation (nephritis), and neurological symptoms.
Idiopathic thrombocytopenic purpura (ITP)
ITP is characterized by a low platelet count due to the immune system mistakenly attacking and destroying platelets.
This immune-mediated destruction of platelets can lead to increased bruising, petechiae, and, in severe cases, spontaneous bleeding.
The cause of ITP is often unknown (idiopathic), although it can sometimes occur secondary to other conditions such as infections, autoimmune diseases, or medications.
How are microangiopathic diseases diagnosed and treated?
Thrombotic thrombocytopenic purpura (TTP) is diagnosed based on clinical symptoms, laboratory tests showing thrombocytopenia, microangiopathic hemolytic anemia, and often reduced activity of the enzyme ADAMTS13. Treatment typically involves plasma exchange (plasmapheresis) to remove antibodies or other factors causing the enzyme deficiency, along with corticosteroids and immunosuppressive drugs.
Hemolytic uremic syndrome (HUS) is diagnosed based on similar criteria, often following a diarrheal illness, and management primarily consists of supportive care, including fluid management and dialysis if necessary. Disseminated intravascular coagulation (DIC) diagnosis relies on clinical symptoms and abnormal clotting parameters, with treatment focusing on addressing the underlying cause and supportive care, including blood transfusions and management of organ dysfunction.
Scleroderma is diagnosed based on clinical symptoms and may involve skin thickening and internal organ involvement, managed through symptomatic treatment and medications targeting specific complications. Diabetic microangiopathy diagnosis involves identifying symptoms like vision changes and kidney dysfunction, managed through blood sugar control and complication management.
Cerebral microangiopathy diagnosis relies on clinical symptoms and neuroimaging studies, with management targeting risk factors for cerebrovascular disease. Systemic lupus erythematosus (SLE) diagnosis includes clinical symptoms and autoantibody testing, managed through a combination of medications to control inflammation and symptom management.
Idiopathic thrombocytopenic purpura (ITP) diagnosis is based on clinical symptoms and a low platelet count, with treatment options ranging from observation to immunosuppressive therapies depending on symptom severity. Multidisciplinary care involving various medical specialties is crucial for comprehensive evaluation and management, with patient education and regular follow-up essential for optimizing outcomes.
Final Words
Understanding microangiopathic diseases like TTP, HUS, and diabetic microangiopathy is important for staying healthy. By knowing their types, symptoms, and how they’re diagnosed and treated, we can take better care of ourselves. Managing these conditions helps prevent complications and improves our overall well-being. So, it’s essential to learn about them and work with healthcare professionals to stay healthy.