Diabetic microangiopathy is a complication of diabetes that damages small blood vessels, leading to issues such as retinopathy, nephropathy, and neuropathy. High blood sugar, advanced glycation end-products, inflammation, and oxidative stress contribute to this condition. Retinopathy affects vision, nephropathy impairs kidney function, and neuropathy causes nerve damage and pain.
Prevention and management focus on glycemic control, blood pressure and lipid management, lifestyle modifications, and regular monitoring. Maintaining blood sugar levels, exercising, eating a healthy diet, and avoiding smoking are crucial. Early detection through routine screenings is essential for timely intervention and to slow the progression of microvascular complications.
Understanding Microangiopathy
Microangiopathy is when small blood vessels in the body, like capillaries, arterioles, and venules, have problems. It’s a big deal for people with diabetes because it causes complications. To understand it better, we need to look at how it happens, what it does to the body, and how it affects people with diabetes.
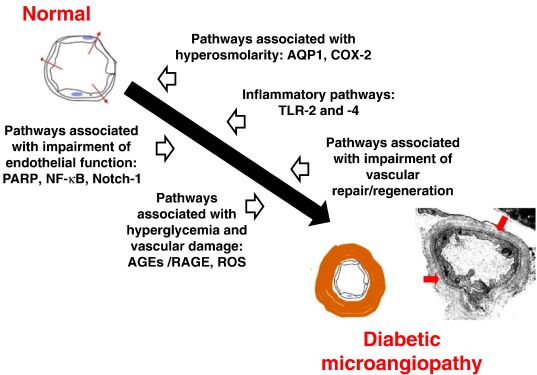
How Microangiopathy Happens
In diabetes, microangiopathy comes from changes caused by having high blood sugar for a long time:
Damage from High Blood Sugar: When blood sugar levels are high, they make things called advanced glycation end-products (AGEs). These AGEs build up on proteins and fats, messing up how they work. This hurts the cells lining the small blood vessels, making them leaky and not work well.
Oxidative Stress: High sugar levels also make the body produce more reactive oxygen species (ROS). These are like little troublemakers that damage the cells lining the blood vessels, causing inflammation and more damage.
Inflammation: High blood sugar makes the body inflamed, which makes the blood vessels even worse. It also makes it easier for certain types of cells to stick to the blood vessel walls, causing more damage.
Blood Flow and Clotting Changes: Diabetes messes up how blood flows and makes it more likely to clot. This can block small blood vessels, stopping blood from reaching tissues and causing damage.
What Microangiopathy Does:
Microangiopathy mostly hurts three important parts of the body in people with diabetes: the eyes, kidneys, and nerves. Here’s what it does to each:
Eyes
Non-Proliferative Diabetic Retinopathy: Causes tiny bulges, bleeding, and fluid buildup. As it gets worse, it can lead to swelling in the center of the vision and vision loss.
Proliferative Diabetic Retinopathy: Makes new, weak blood vessels in the eye that can bleed into the eye, causing severe vision problems.
Kidneys
- Microalbuminuria: Early sign of kidney damage, shows up as small amounts of protein in the urine.
- Proteinuria: As kidney damage gets worse, more protein leaks into the urine.
- Reduced Kidney Function: In later stages, the kidneys don’t work well, leading to kidney failure.
Nerves
- Peripheral Neuropathy: Causes numbness, pain, and loss of feeling in the hands and feet.
- Autonomic Neuropathy: Affects things like digestion and heart rate, causing problems like slow digestion and low blood pressure.
How to Find Microangiopathy Early?
Finding microangiopathy early is crucial to preventing severe complications. Regular check-ups are essential for this purpose. For the eyes, it is important to have an annual eye examination to detect any early signs of retinopathy. For the kidneys, routine urine tests can help identify early stages of kidney damage, such as microalbuminuria. Additionally, regular foot examinations and tests to assess nerve function are necessary to detect neuropathy.
Specialized tests can also play a significant role in early detection. Optical Coherence Tomography (OCT) provides detailed images of the eyes, allowing for the identification of retinal issues. Renal ultrasound is used to assess the kidneys for any structural damage. Researchers are also exploring the use of biomarkers—specific indicators in the body—that can signal early damage to small blood vessels. By utilizing these screening methods and tests, it is possible to catch microangiopathy early and take steps to manage it effectively.
How to Manage and Prevent Microangiopathy?
Managing and preventing microangiopathy involves controlling blood sugar, blood pressure, and addressing any complications. Effective management starts with maintaining normal blood sugar levels through insulin or other medications, aiming for a level below 7%. Blood pressure control is also crucial; medications such as ACE inhibitors or ARBs can help keep it within a normal range.
Managing cholesterol levels is equally important, as lowering cholesterol can benefit the heart and blood vessels. Additionally, specific treatments are available for various complications. For the eyes, laser treatments or injections can mitigate retinopathy. For the kidneys, certain medications can slow the progression of kidney damage. For nerve-related issues, pain management and diligent foot care are essential to prevent further complications. By focusing on these areas, individuals can effectively manage and prevent the progression of microangiopathy.